Eye health
Your eyes are among your most precious assets, yet many vision-threatening conditions develop silently, without obvious warning signs. From the refractive errors affecting billions worldwide to sight-stealing diseases like glaucoma and macular degeneration, understanding the landscape of eye health empowers you to take meaningful action before problems become irreversible.
This comprehensive resource introduces the major categories of eye conditions you should understand—how they develop, why certain populations face higher risks, and what practical steps you can take today to protect your vision for decades to come. Whether you’re navigating the myopia epidemic affecting younger generations, managing a diagnosed condition, or simply seeking to maintain healthy eyes, the knowledge you gain here will serve as your foundation for informed decisions and proactive care.
Understanding Refractive Errors and Vision Clarity
Refractive errors represent the most common reason people experience blurred vision, affecting nearly 2.6 billion people globally. These conditions occur when the eye’s optical system—the cornea and lens—fails to focus light precisely on the retina, creating images that appear fuzzy or distorted at certain distances.
The Four Main Types and Their Characteristics
Myopia (nearsightedness) makes distant objects appear blurry while near vision remains clear. Hyperopia (farsightedness) creates the opposite pattern, though many younger people can compensate temporarily through muscular effort that often leads to eye strain. Astigmatism produces distorted vision at all distances due to an irregularly shaped cornea, while presbyopia—the age-related loss of focusing flexibility—typically begins affecting reading vision around the mid-forties.
Why These Errors Change Throughout Your Life
Your eyes aren’t static organs. Childhood myopia often progresses as the eyeball continues growing longer than optimal. Conversely, some mild hyperopia in youth becomes more noticeable as the lens loses elasticity with age. Think of your eye’s lens like a camera’s autofocus mechanism—when new, it adjusts effortlessly, but decades of use gradually diminish its range of motion. This is why someone who never needed glasses at twenty-five might suddenly struggle with restaurant menus at forty-five.
The Hidden Cost of “Minor” Refractive Problems
Many people dismiss slight blur as insignificant, but uncorrected refractive errors create cascading effects. Students may struggle academically not due to learning difficulties but simply because they can’t see the board clearly. Adults experience headaches, eye fatigue, and reduced productivity. Even a seemingly small prescription can reduce quality of life by 15-20% through accumulated visual stress throughout the day.
The Growing Myopia Challenge
Myopia has reached epidemic proportions, with projections suggesting that half the world’s population may be nearsighted within coming decades. This isn’t merely about needing glasses—high myopia significantly increases risks for serious conditions like retinal detachment, glaucoma, and macular degeneration later in life.
Modern Lifestyles as the Primary Accelerator
Our ancestors spent considerably more time outdoors with eyes focused on distant horizons. Today’s children and adults spend hours with screens and books held at arm’s length or closer. Research consistently shows that less than 90 minutes of daily outdoor time correlates strongly with myopia development. The eye appears to elongate in response to prolonged near-focus demands—an adaptation that permanently alters its optical properties.
Practical Interventions That Make a Difference
For children, implementing the 20-20-20 rule creates essential visual breaks: every 20 minutes of near work, look at something 20 feet away for 20 seconds. This simple habit allows focusing muscles to relax and may slow progression. Optimizing study environments with proper lighting, appropriate viewing distances, and regular outdoor play provides additional protection. Specialized myopia control lenses and orthokeratology (overnight reshaping lenses) offer more aggressive intervention for high-risk children, potentially reducing progression by 30-60% compared to standard correction.
Glaucoma: Protecting Your Peripheral Vision
Often called the “silent thief of sight,” glaucoma damages the optic nerve—typically through elevated intraocular pressure—gradually stealing peripheral vision so subtly that many patients don’t notice until significant irreversible loss has occurred. By the time someone perceives vision changes, up to 40% of nerve fibers may already be destroyed.
Beyond Pressure: Understanding Multiple Risk Factors
While elevated eye pressure remains the primary modifiable risk factor, it’s not the complete story. Some people develop glaucoma with normal pressure readings, while others tolerate high pressure without damage. Age over sixty, family history, certain ethnic backgrounds, extreme nearsightedness, and thin corneas all contribute to individual risk profiles. This complexity explains why screening requires more than a simple pressure check—comprehensive evaluation includes optic nerve examination and visual field testing.
The Critical Importance of Treatment Adherence
Glaucoma medications—typically daily eye drops—work by reducing intraocular pressure to slow or halt nerve damage. Here’s the challenge: because glaucoma rarely causes symptoms in early stages, patients often discontinue treatment when they feel fine. This represents a critical error. Think of glaucoma drops like blood pressure medication—the absence of symptoms doesn’t mean the threat has disappeared. Stopping treatment allows pressure to rise again, permitting continued nerve destruction that cannot be reversed.
Corneal Health and Infection Prevention
Your cornea—the clear dome covering the front of your eye—serves as both a protective barrier and a critical optical element. When bacteria, fungi, or parasites breach this barrier, the resulting keratitis (corneal infection) can rapidly progress from minor irritation to vision-threatening emergency within 24-48 hours.
Contact Lens Wearers Face Elevated Risks
Contact lenses create an environment where organisms can thrive against the corneal surface. Pseudomonas aeruginosa—a bacterium found in water sources—represents the lens wearer’s particular nemesis, capable of causing devastating infections with remarkable speed. Swimming, showering, or even rinsing lenses in tap water introduces this threat. The classic warning sign is a painful white or gray spot on the cornea accompanied by redness, light sensitivity, and discharge.
Prevention Through Rigorous Hygiene
Preventing corneal infections requires consistent habits:
- Never expose lenses to any water source—only use fresh sterile solution
- Replace lenses and cases according to prescribed schedules
- Wash hands thoroughly before handling lenses
- Remove lenses immediately if eyes become red or uncomfortable
- Never sleep in lenses unless specifically prescribed for extended wear
When symptoms appear, timing matters critically. Same-day ophthalmologic evaluation can mean the difference between successful treatment and permanent scarring.
Managing Dry Eye Syndrome
Dry eye affects millions, creating sensations of grittiness, burning, or paradoxically, excessive watering as eyes attempt to compensate for inadequate lubrication. The condition arises when tear production decreases or when tears evaporate too quickly—often both factors contribute simultaneously.
The Anatomy of Your Tear Film
Healthy tears aren’t simply water—they consist of three distinct layers. The innermost mucin layer helps tears adhere to the eye surface. The middle aqueous layer provides hydration and delivers nutrients. The outer lipid layer, secreted by Meibomian glands along the eyelid margins, prevents rapid evaporation. When these glands become blocked or dysfunctional—often from inflammation or age—tears evaporate in seconds rather than maintaining adequate coverage.
Modern Environmental Aggressors
Contemporary life bombards eyes with drying factors. Computer use reduces blink rates from a normal 15-20 times per minute to as few as 5-7 times, limiting tear distribution. Air conditioning, heating systems, and ceiling fans create convective airflow that accelerates evaporation. Certain medications, including antihistamines and antidepressants, reduce tear production as a side effect.
Practical Solutions and Therapeutic Approaches
Simple blink exercises—consciously performing 10-15 complete, gentle blinks every hour—help redistribute tears and stimulate gland function. Positioning screens below eye level reduces exposed eye surface area. Warm compresses applied to closed eyelids for 5-10 minutes daily can soften blocked Meibomian gland secretions. For moderate to severe cases, prescription anti-inflammatory drops, punctal plugs (which reduce tear drainage), or in-office procedures to clear gland blockages may be necessary.
Early Detection: Your First Line of Defense
Many serious eye diseases progress asymptomatically for months or years. Your brain remarkably compensates for gradual vision loss—filling in blind spots, adapting to reduced contrast sensitivity, and adjusting to subtle changes that would alarm you if they occurred suddenly. This adaptive capability, while impressive, works against early detection of conditions best treated in their initial stages.
Home Monitoring Tools Anyone Can Use
The Amsler grid—a simple pattern of straight lines with a central dot—provides an effective method for detecting macular changes. When viewed with one eye at a time at reading distance, any lines appearing wavy, distorted, or missing suggest potential macular problems requiring professional evaluation. This two-minute weekly self-check can identify issues like macular degeneration or macular edema before they significantly impact daily function.
Recognizing the Difference Between Chronic and Acute Symptoms
Gradual changes—slowly increasing blur, slight color desaturation, or minor peripheral vision loss—often indicate chronic conditions requiring scheduled professional attention. Acute symptoms demand immediate care:
- Sudden vision loss or dramatic vision reduction
- New floaters, especially accompanied by flashes of light
- Curtain or shadow appearing in peripheral vision
- Severe eye pain with vision changes
- Sudden onset of double vision
Family History as a Risk Amplifier
Glaucoma, macular degeneration, and certain retinal conditions show strong hereditary patterns. If a first-degree relative has been diagnosed with these conditions, your risk increases four to nine times compared to the general population. This doesn’t guarantee you’ll develop the condition, but it does warrant earlier and more frequent screening—often beginning a decade before the typical age of onset.
Age-Related Macular Degeneration: Preserving Central Vision
Age-related macular degeneration (AMD) affects the macula—the retina’s central region responsible for sharp, detailed vision used in reading, driving, and recognizing faces. As the leading cause of severe vision loss in people over sixty, AMD progresses through stages from early changes barely affecting vision to advanced forms causing significant central vision loss.
Understanding Drusen and Disease Progression
AMD typically begins with drusen—yellow deposits of cellular waste products accumulating beneath the retina. Small, scattered drusen may remain stable for years without vision impact. Larger or more numerous drusen indicate higher progression risk. Think of drusen like rust forming on metal—a few spots may be cosmetic, but widespread accumulation signals structural compromise. Advanced AMD takes two forms: “dry” AMD with gradual cell death, and “wet” AMD where abnormal blood vessels leak fluid and blood under the retina, causing rapid vision loss.
Nutritional Defense and the AREDS Formulas
Landmark research established that specific high-dose antioxidant and mineral supplementation—the AREDS formula—reduces progression risk by approximately 25% in people with intermediate or advanced AMD in one eye. The updated AREDS2 formula substituted lutein and zeaxanthin for beta-carotene (which increased lung cancer risk in smokers) and reduced zinc dosage. While these supplements don’t prevent AMD or restore lost vision, they represent meaningful intervention for at-risk individuals.
Lifestyle Factors Within Your Control
Beyond supplementation, several modifiable factors influence AMD risk. Smoking doubles or triples risk and accelerates progression—cessation at any age provides benefit. Decades of cumulative UV exposure damages retinal cells, making quality sunglasses with UV protection a worthwhile investment throughout life. Cardiovascular health correlates with retinal health; factors promoting heart disease (hypertension, poor diet, sedentary lifestyle) similarly threaten macular function.
When Injections Become Necessary
For wet AMD, anti-VEGF injections—medications injected directly into the eye to stop abnormal blood vessel growth—have revolutionized treatment. While the prospect of eye injections understandably causes anxiety, these procedures are performed with anesthetic and have preserved or improved vision for millions who would have faced inevitable severe vision loss just decades ago. Treatment timing proves critical—the sooner wet AMD is detected and treated, the better the visual outcome.
Protecting your vision requires understanding both the threats your eyes face and the practical actions that mitigate these risks. From encouraging children to play outdoors to adhering faithfully to glaucoma medications, from never swimming in contact lenses to monitoring your vision with an Amsler grid, small consistent actions compound into significant long-term protection. Your eyes change throughout your life, and your care approach should evolve accordingly—what your eyes need at twenty differs from what they require at fifty or seventy. By staying informed and proactive, you give yourself the best opportunity for clear, functional vision throughout your lifetime.

Dry AMD or Wet AMD: Which Diagnosis Offers More Treatment Options?
While wet AMD has more direct medical treatments, understanding both forms of macular degeneration is the key to actively preserving your vision and turning fear into empowerment. Dry AMD involves cellular waste buildup (drusen) and is primarily managed with proactive…
Read more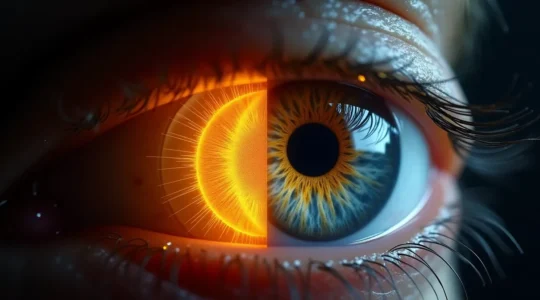
Glaucoma or Hypertension: Which Silent Killer Strikes the Eyes First?
The greatest risk to your sight isn’t a disease, but the false sense of security created by your own brain, which actively hides evidence of damage. Vision loss from glaucoma often begins silently in the periphery, with your brain creating…
Read more
Evaporative vs. Aqueous Deficient Dry Eye: A Diagnostic Guide for Chronic Sufferers
Chronic dry eye that doesn’t respond to standard drops is often a sign of a mechanical failure in your tear system, not just a lack of moisture. Evaporative Dry Eye (EDE), accounting for 86% of cases, is a plumbing issue…
Read more
Red Eye or Ulcer: How to Tell if Your Infection Is Dangerous?
That painful red eye isn’t just ‘contact lens irritation’—it could be a fast-moving infection capable of causing permanent vision loss in as little as 24 hours. Aggressive bacteria like Pseudomonas don’t just infect; they release enzymes that literally melt corneal…
Read more
Open-Angle or Closed-Angle: Which Glaucoma Type Is a Medical Emergency?
Most people think of glaucoma as a slow, silent disease—a dangerously incomplete picture. The critical distinction is that only one type constitutes a true medical emergency that can cause blindness in hours. Open-Angle Glaucoma: This is the “silent thief.” It…
Read more
Is Your Child’s Nearsightedness Progressing Too Fast for Standard Glasses?
Contrary to common belief, stronger glasses are a temporary fix, not a solution for childhood myopia; they fail to address the underlying disease progression that increases the risk of permanent vision loss. Myopia is driven by the physical stretching of…
Read more
Astigmatism, Hyperopia, or Presbyopia: What Causes Your Blurry Text?
The frustration of blurry text is often caused by three distinct refractive errors, but the key to identifying yours lies in understanding *when* and *how* the blur appears. Blur that worsens with prolonged close work and causes headaches often signals…
Read more