
Contrary to common belief, stronger glasses are a temporary fix, not a solution for childhood myopia; they fail to address the underlying disease progression that increases the risk of permanent vision loss.
- Myopia is driven by the physical stretching of the eye (axial elongation), a process that standard glasses do not stop.
- Each -1.00 diopter of progression significantly raises the lifetime risk of sight-threatening conditions like retinal detachment.
Recommendation: Shift from reactive correction to proactive management with proven strategies like myopia control lenses, behavioral changes, and environmental optimization to protect your child’s future sight.
As a parent, you’ve likely felt a growing sense of unease with each eye exam. Your child’s prescription for nearsightedness gets stronger, the lenses get thicker, and you wonder where it will end. The conventional approach is simple: update the glasses and move on. This cycle feels normal, almost expected. We are told to limit screen time and encourage outdoor play, but these recommendations often feel vague and difficult to enforce, leaving parents feeling powerless as the numbers on the prescription chart continue to climb.
But what if this entire framework is wrong? What if we’ve been taught to treat myopia as a simple inconvenience—a refractive error—when it is, in fact, a progressive disease with serious, irreversible consequences? The relentless worsening of your child’s vision isn’t just about needing stronger glasses; it’s a symptom of a physical change in the eye itself. The eyeball is elongating, stretching the delicate retinal tissue thinner and thinner with each passing year. This is the critical piece of information that is often lost in routine eye appointments.
This article will reframe your understanding of childhood myopia. We are moving beyond reactive correction and into the realm of proactive disease management. The goal is not merely to help your child see clearly today, but to actively slow the progression of their myopia to protect their eyes from potentially devastating, sight-threatening conditions tomorrow. We will explore the science behind why this is happening, the concrete risks associated with every diopter of change, and the powerful, evidence-based strategies you can implement right now to take control. This is not about blame; it’s about empowerment. The time to act is now.
This guide provides a structured path to understanding and managing your child’s myopia. Below, you will find a summary of the key areas we will cover, from environmental risk factors to the specifics of advanced treatment options.
Summary: A Parent’s Guide to Halting Myopia Progression
- Why Indoor Playtime Increases Myopia Risk by 30% in School-Aged Children?
- How to Gamify Eye Breaks so Children Actually Follow Them?
- Standard Lenses or Myopia Control: Which Is Worth the Investment for a 10-Year-Old?
- The Retinal Detachment Risk That Spikes With Every -1.00 Diopter Increase
- Problem & Solution: Setting Up a Myopia-Friendly Homework Station
- Why Your Vision Reverts if You Skip Ortho-K Lenses for 2 Nights?
- Why Focusing Close for Too Long Locks Your Focus Muscle?
- Is Ortho-K Safe for Children to Control Myopia Progression?
Why Indoor Playtime Increases Myopia Risk by 30% in School-Aged Children?
The advice to “go play outside” is common, but it’s rarely explained with the urgency it deserves. This isn’t just about general well-being; it’s a critical medical intervention for your child’s eyes. The core issue is not the activity itself, but the intensity of light. The typical indoor environment, even in a brightly lit room, provides around 500 lux of light. In contrast, being outdoors, even on an overcast day, exposes the eyes to over 10,000 lux. This dramatic difference in brightness is the key.
Scientific evidence strongly suggests that bright, natural light stimulates the release of dopamine in the retina. This neurotransmitter acts as a crucial “stop signal,” inhibiting the abnormal growth and elongation of the eyeball (axial elongation) that defines myopia progression. Insufficient exposure to this bright light effectively removes the brakes on eye growth. A landmark Shanghai study, the STORM trial, used smartwatches to track children and found that spending an average of 90 minutes outdoors daily, with sustained exposures to light over 2,000 lux, significantly reduced myopic shift. The evidence is overwhelming: time spent indoors starves the eye of the one natural element proven to protect it.

As the image above illustrates, the disparity between indoor and outdoor lighting is not subtle. It’s a fundamental environmental factor. Research confirms the power of this intervention; a 2024 meta-analysis shows that children with the highest outdoor time had a 53% reduction in myopia onset risk compared to those with the least. Every hour spent indoors during daylight is a missed opportunity to actively defend your child’s vision. Prioritizing outdoor time isn’t just a nice idea—it’s an essential component of their visual hygiene.
How to Gamify Eye Breaks so Children Actually Follow Them?
While insufficient outdoor light promotes eye elongation, prolonged near-work actively strains the focusing system. When a child stares at a book or screen, their ciliary muscle contracts to focus up close. Hours of this sustained contraction can lead to a state of “lock-in,” known as accommodative spasm, where the muscle struggles to relax and see clearly at a distance. This is why your child might complain of blurry vision when looking up from homework. To combat this, a structured routine of eye breaks is non-negotiable.
The most validated method is the 20-20-20 rule, a concept strongly endorsed by eye care professionals. As the American Academy of Ophthalmology explains, the principle is simple and effective:
Every 20 minutes, focus your eyes on an object at least 20 feet away for at least 20 seconds.
– American Academy of Ophthalmology, WebMD – Myopia: How to Slow Progression in Your Child
However, telling a child to follow this rule is often ineffective. The key to compliance is to transform this clinical instruction into a series of engaging games. By “gamifying” the process, you can build a consistent habit of visual hygiene without constant nagging. Instead of a chore, eye breaks become a fun, rewarding part of their routine.
Here are several practical strategies to turn the 20-20-20 rule into a game your child will actually want to play:
- Eye Spy Missions: Every 20 minutes, a timer goes off. The mission? “I spy with my little eye… five things that are blue outside the window.” This forces them to look far away and actively search.
- Distance Detective Chart: Create a chart with daily spotting challenges. “Find a bird’s nest,” “Spot a red car,” “Count the windows on the building across the street.” They get a sticker for each completed mission.
- Power-Up Timers: Use a fun timer app that frames breaks as “Eye Power-Ups” or “Focus Recharges.” When the timer rings, it’s time to “level up” their eyes for the next 20 minutes of work.
- The Alphabet Game: Look out the window and find an object that starts with “A,” then “B,” and so on. This keeps them engaged for well over the required 20 seconds.
Standard Lenses or Myopia Control: Which Is Worth the Investment for a 10-Year-Old?
When your 10-year-old’s vision worsens, the default solution is a new pair of standard single-vision glasses. This is a classic example of reactive correction: the glasses help them see clearly now but do absolutely nothing to stop the underlying disease from progressing. In fact, some evidence suggests that standard lenses, by creating peripheral hyperopic defocus, may even accelerate eye growth. The alternative is proactive management, using specialized lenses or treatments designed to slow or halt the progression of myopia.
This decision point often comes down to cost. Myopia control options—such as MiSight contact lenses, Orthokeratology (Ortho-K), or Atropine eye drops—are significantly more expensive upfront than a standard pair of glasses. It’s natural for a parent to question if the investment is worthwhile. To answer this, we must shift the perspective from a short-term expense to a long-term investment in your child’s future health and quality of life. The higher initial cost is buying a reduction in future risk.
These treatments are highly effective. For instance, clinical trials of MiSight contact lenses demonstrated that 41% of eyes showed no progression over a three-year period. This isn’t just about avoiding thicker glasses; it’s about keeping your child in a lower-risk category for life-altering eye diseases. The financial and personal cost of treating retinal detachment or glaucoma later in life far outweighs the investment in myopia control today. The following table breaks down the 10-year financial and clinical implications, reframing the choice not as a purchase, but as a strategic health decision.
| Treatment Option | Annual Cost | 10-Year Total | Myopia Progression Rate | Long-term Benefits |
|---|---|---|---|---|
| Standard Single Vision Glasses | $200-400 | $2,000-4,000 | -0.50 to -0.75D/year | Vision correction only |
| MiSight Contact Lenses | $1,200-1,800 | $12,000-18,000 | 59% slower progression | Reduced risk of high myopia complications |
| Ortho-K Lenses | $1,500-2,500 | $15,000-25,000 | 50% slower progression | Daytime freedom from glasses |
| Atropine Drops + Glasses | $600-1,000 | $6,000-10,000 | 30-50% slower progression | Lower cost myopia control option |
The Retinal Detachment Risk That Spikes With Every -1.00 Diopter Increase
The most critical concept for any parent of a myopic child to understand is this: myopia is not a benign condition. The true danger lies in the axial elongation—the physical stretching of the eyeball. Imagine a balloon being slowly inflated over many years. As it stretches, its walls become thinner, weaker, and more fragile. The same thing happens to the retina, the light-sensitive tissue at the back of the eye. This progressive thinning dramatically increases the lifetime risk of catastrophic, sight-threatening events.
The most terrifying of these is retinal detachment, a medical emergency where the retina pulls away from its underlying tissue, leading to permanent vision loss if not treated immediately. This is not a risk reserved for the “severely” myopic. The danger accumulates with every single diopter of progression. Recent research highlights this alarming correlation, showing a 10% increased odds of retinal detachment per diopter increase. A child who progresses from -2.00D to -5.00D has not just worsened their vision; they have significantly multiplied their lifetime risk of blindness.
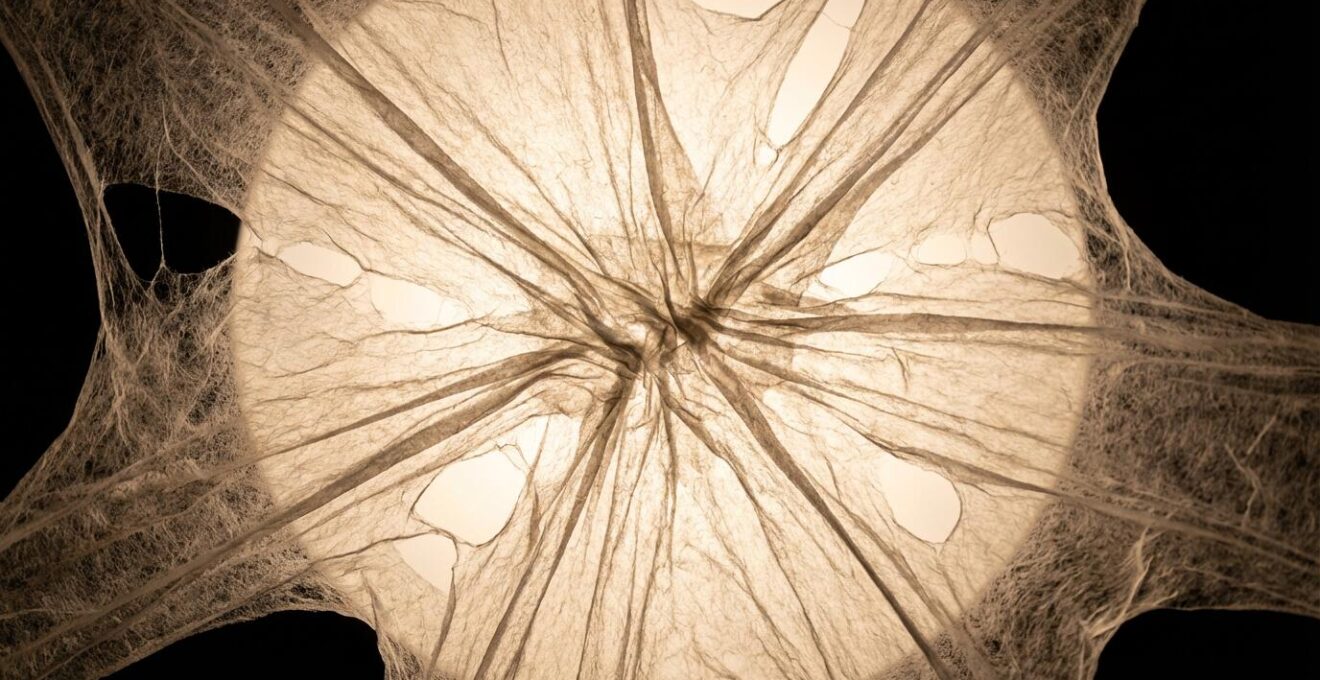
The visual above conceptualizes the physical stress on the retina. This stretching creates weak spots and tears, predisposing the eye to detachment. The numbers from clinical studies are stark and should serve as a wake-up call for every parent. The risk is not linear; it’s exponential.
Case Study: The Exponential Risk Multiplier of Myopia
The landmark Eye Disease Case-Control Study quantified the frightening reality of this risk progression. Compared to a non-myopic individual, a person with mild myopia (-1.00D to -3.00D) already has a 4-fold increased risk of retinal detachment. For those with moderate myopia (worse than -3.00D), that risk jumps to 10 times higher. For high myopes (often defined as -6.00D or more), the risk skyrockets to a staggering 20 to 40 times that of a healthy eye. Every diopter you prevent in childhood directly lowers your child’s position on this terrifying ladder of risk.
Problem & Solution: Setting Up a Myopia-Friendly Homework Station
While outdoor time and eye breaks are crucial, the environment where your child spends hours doing near-work is a major battleground in the fight against myopia. A poorly configured homework station forces the eyes to work harder, increasing strain on the ciliary muscle and potentially contributing to accommodative spasm and progression. The American Academy of Ophthalmology notes that while a direct link isn’t proven, research suggests that children who spend more time indoors doing near-focused activities have higher rates of myopia. Optimizing this space is a simple, high-impact intervention you can implement today.
The goal is to create a station that minimizes eye strain by controlling three key factors: working distance, viewing angle, and lighting. The common habit of a child hunching over a book flat on a desk is one of the worst-case scenarios, forcing their eyes to focus at an extremely close distance and an awkward angle. By making a few simple adjustments, you can establish an ergonomically sound and visually hygienic workspace.
Think of it as setting up a professional workstation for your child. These are not just suggestions; they are ergonomic principles designed to protect their developing visual system. Here is a checklist to audit and correct your child’s homework setup:
- Establish the Harmon Distance: The ideal working distance from the eyes to the book or screen is the distance from their elbow to their middle knuckle. Have them make a fist and place their elbow on the desk; the book should be where their knuckles are. This is a non-negotiable minimum distance.
- Adjust Chair and Posture: The chair height should allow their feet to be flat on the floor, with their thighs parallel to the ground. This stable posture prevents them from hunching forward.
- Set the Gaze Angle: Reading material or screens should be propped up on a book stand or monitor arm to create a 20-degree downward gaze angle. This is the most relaxed position for the eyes and neck.
- Optimize Lighting: The main light source should come from the side, not from behind (which creates a shadow) or directly in front (which creates glare). Ensure the work surface itself is illuminated with at least 500 lux, which is brighter than typical room lighting. Use a dedicated desk lamp.
- Enforce Minimum Distance: A hard rule should be that no screen or reading material ever comes closer than 16 inches (40cm) from their eyes.
Why Your Vision Reverts if You Skip Ortho-K Lenses for 2 Nights?
Orthokeratology, or Ortho-K, is a powerful myopia management tool where a child wears rigid, gas-permeable contact lenses overnight. These lenses act as corneal molds, gently and temporarily reshaping the front surface of the eye while they sleep. The result is clear vision throughout the day without the need for glasses or contact lenses. However, this effect is entirely reversible, and understanding why is key to ensuring compliance and success with the treatment.
The cornea is an elastic tissue. The Ortho-K lens applies gentle hydraulic pressure via the tear film to flatten the central cornea, correcting the refractive error. When the lens is removed in the morning, the cornea holds this new shape for the day. But this is not a permanent change. As practitioners at Lurie Children’s Hospital explain, if you stop wearing the lenses, the cornea’s natural elasticity causes it to gradually return to its original, myopic shape. This regression is not a failure of the treatment; it is proof that it’s working as a temporary, non-invasive molding process.
The timeline for this reversion is rapid. After missing just one night of wear, a child might maintain clear vision for most of the morning but notice blurriness creeping in by late afternoon. After missing two consecutive nights, the effect is almost completely gone. Their morning vision will be nearly as blurry as it was before they ever started treatment. This is why consistent, nightly wear is non-negotiable for Ortho-K to be effective both for vision correction and, more importantly, for its intended purpose of slowing myopia progression. It functions like a dental retainer after braces: skip it, and the structure reverts.
Why Focusing Close for Too Long Locks Your Focus Muscle?
The human eye is not designed for the modern childhood. It evolved for a world where we predominantly looked at distant objects, with only brief periods of near focus. Today, that is completely inverted. With CDC estimates showing children ages 8-10 spend 6 hours per day on screens for entertainment alone, not including schoolwork, their eyes are held in a state of near-focus for unprecedented lengths of time. This chronic overuse has a direct physical consequence on the eye’s focusing muscle, the ciliary body.
When you look at something up close, the ciliary muscle contracts. This allows the eye’s natural lens to become more convex, increasing its focusing power. When you look far away, the muscle is supposed to relax completely. The problem is that after hours of sustained contraction, this muscle can develop a cramp, much like any other overworked muscle in your body. This condition, known as accommodative spasm or “focus lock,” means the muscle struggles to relax even when the child looks up to see something in the distance. The result is temporarily blurred distance vision, eye strain, and headaches.
While often temporary, chronic accommodative spasm is a significant red flag. It is a key factor in eye fatigue and discomfort and is believed by many experts to be a contributing factor to the progression of myopia. As a parent, you are on the front lines of spotting this problem. You must become an active observer of your child’s visual behaviors and complaints, as they are often the first signs that their visual system is under duress. Recognizing these symptoms early allows for immediate intervention, primarily through enforcing the structured eye breaks discussed earlier.
Here are the key symptoms of accommodative spasm to watch for:
- Complaints of Blurry TV: The most classic sign. Their vision is blurry when looking up from a book or tablet to watch TV across the room.
- Frequent Eye Rubbing: A physical attempt to relieve the strain and discomfort of the locked muscle.
- Tension Headaches: Often centered around the eyes or forehead, especially after long periods of reading or homework.
- Aversion to Near Work: The child may start to avoid reading because they subconsciously associate it with discomfort.
Key Takeaways
- Myopia is a progressive disease of eye elongation, not just a refractive error that needs stronger glasses.
- Every diopter of progression exponentially increases the lifetime risk of irreversible, sight-threatening conditions like retinal detachment.
- Proactive management through myopia control lenses, increased outdoor time (for light exposure), and strict visual hygiene is a medical necessity, not an option.
Is Ortho-K Safe for Children to Control Myopia Progression?
For any parent considering a medical treatment for their child, safety is the primary concern. The idea of a child wearing contact lenses overnight can be intimidating. It is essential to approach the question of Ortho-K safety with facts, not fear. When prescribed and managed by a qualified and experienced practitioner, Ortho-K is a remarkably safe and effective method for myopia control in children.
The main risk associated with any contact lens wear, including Ortho-K, is microbial keratitis, a serious infection of the cornea. However, the risk is extremely low when proper hygiene protocols are followed. Data shows that the risk of infection with Ortho-K is approximately 1-2 cases per 10,000 wearers per year. While this is not zero, it is comparable to the risks associated with other overnight contact lens modalities and can be minimized through meticulous cleaning, proper handling, and vigilant parental supervision, especially in younger children.
The safety of the treatment is fundamentally tied to the expertise of the practitioner and the diligence of the family. A successful Ortho-K journey is a partnership. The practitioner’s role is to ensure a perfect, custom fit using advanced tools like a corneal topographer and to provide a clear protocol for follow-up and emergencies. Your role as a parent is to enforce strict hygiene, supervise lens insertion and removal until your child is proficient, and watch for any red-flag symptoms like pain, persistent redness, or a sudden change in vision. Choosing the right practitioner is the single most important safety decision you will make.
Your Action Plan: Vetting an Ortho-K Practitioner
- Identify Potential Providers: List local optometrists certified in myopia management and Ortho-K. Ask about their experience specifically with pediatric patients.
- Gather Protocol Documents: Request their standard follow-up schedule for the first month and their written emergency contact procedures. A professional clinic will have these readily available.
- Assess the Training Process: Inquire about their training plan for lens insertion, removal, and cleaning. Ensure it is hands-on and that they won’t dispense lenses until both you and your child are confident.
- Confirm Critical Red Flags: Ask the practitioner to explicitly list the red-flag symptoms (e.g., pain, light sensitivity, discharge) that require immediate contact, and what to do if they occur after hours.
- Finalize the Safety Plan: Choose the practitioner who provides the most comprehensive and confidence-inspiring safety protocol, and schedule the initial fitting and all required follow-up appointments.
By reframing myopia as a manageable disease, you are taking the most important step toward protecting your child’s long-term eye health. The next step is to partner with an eye care professional who specializes in myopia management to create a personalized treatment plan.
Frequently Asked Questions About Ortho-K and Myopia Control
Is the vision reversion after skipping Ortho-K dangerous?
No, the regression is not dangerous and is actually proof the treatment is working. It shows the cornea is elastic and the effect is temporary, similar to a dental retainer after braces. This reversibility is a key safety feature of the treatment.
How quickly does vision return after stopping Ortho-K?
Vision begins reverting within 24 hours, with significant blur after 48 hours. Complete return to the original prescription typically occurs within 1-2 weeks of discontinuing wear, with no permanent change to the eye’s structure.
Can I skip Ortho-K occasionally without consequences?
Occasional single-night skips may be manageable for some, but will likely result in blurred vision the following afternoon. For consistent, clear daytime vision and the all-important myopia control benefit, nightly wear is essential and should be the goal.