
The choice is not just MIGS vs. Trabeculectomy; it’s about understanding the entire surgical ecosystem designed for your safety and recovery.
- Modern eye surgery relies on patient-centric anesthesia, allowing you to be awake but comfortable for a quicker, safer recovery.
- Advanced technologies like robotics and lasers provide unprecedented precision, minimizing tissue disruption and enhancing surgical outcomes.
- Your recovery is a planned architectural phase, with clear protocols designed to maximize the procedure’s success and your comfort.
Recommendation: Use this guide to move beyond fear and have a more empowered, in-depth conversation with your surgeon about the specific technologies and protocols that will be part of your personal treatment plan.
For a patient diagnosed with glaucoma and facing the prospect of surgery, the primary question often boils down to a single comparison: MIGS or Trabeculectomy? The fear of a traditional, invasive procedure is valid, and the promise of a minimally invasive option with faster recovery is compelling. You’ve likely heard that Minimally Invasive Glaucoma Surgery (MIGS) is the newer, gentler option, while a trabeculectomy is the more powerful, “gold standard” procedure reserved for advanced cases. This comparison, while accurate on the surface, misses the bigger picture and the true source of reassurance.
The real confidence boost doesn’t come from choosing one procedure over the other, but from understanding the sophisticated and interconnected ecosystem of modern ophthalmic surgery. True peace of mind is found in the knowledge that every step—from the way you are kept comfortable during the procedure to the precision of the instruments and the design of your recovery—is engineered for control and safety. The anxiety you feel often stems from the unknown, the fear of losing control. This article aims to replace that fear with knowledge.
We will explore the key pillars of this surgical ecosystem. By demystifying the technology and protocols that surround your procedure, you will see that modern eye surgery is less about a single, intimidating event and more about a controlled, precise, and well-managed process. This understanding will empower you to have a more confident and productive conversation with your surgeon, focusing not just on “which surgery,” but on “how” the entire process is tailored to your safety and long-term vision.
This comprehensive overview will walk you through the critical components of today’s advanced ophthalmic procedures. By exploring each element, you’ll gain a holistic understanding of the safety, precision, and care involved, moving from patient anxiety to informed confidence.
Summary: A Patient’s Guide to the Modern Surgical Ecosystem
- Why You Remain Awake But Numb During Most Eye Surgeries?
- How Robotic Assistance Improves Precision in Retinal Peeling?
- Injections or Surgery: Which Is Best for a Macular Hole?
- The Endophthalmitis Risk: Why Water Is the Enemy After Eye Surgery
- Problem & Solution: Surviving “Face-Down” Recovery Without Neck Pain
- Non-Proliferative or Proliferative: Which Stage Requires Laser Treatment?
- Femtosecond Laser or Manual Incision: Is the Extra Cost Worth the Precision?
- Open-Angle or Closed-Angle: Which Glaucoma Type Is a Medical Emergency?
Why You Remain Awake but Numb During Most Eye Surgeries?
You remain awake during most eye surgeries because modern anesthesia techniques, primarily “twilight sedation” combined with topical anesthetics, provide profound numbness without the risks and extended recovery of general anesthesia. This approach enhances safety by allowing you to communicate if needed, while ensuring you feel no pain. For many patients, the idea of being conscious is a primary source of anxiety, but this method is a cornerstone of modern, patient-centric surgical care.
This technique involves two key components. First, topical anesthetic drops are used to completely numb the surface of the eye. These are highly effective for procedures like glaucoma or cataract surgery that don’t require total paralysis of the eye muscles (akinesia). As a landmark guide from the NCBI explains, this method also mitigates bleeding risks for patients on anticoagulants. Second, an anesthesiologist administers mild intravenous sedation. As experts at UCLA Health note, under this “twilight” state, you are relaxed and drowsy but remain able to respond to simple instructions, giving the surgical team an added layer of real-time feedback.
The most significant benefit for the patient is the recovery. Unlike general anesthesia, which can leave you feeling groggy for many hours, this lighter approach allows for a much faster return to normalcy. In fact, studies on patient recovery show that with twilight sedation, many patients feel ‘back to normal’ by the evening of the surgery. This combination of safety, comfort, and rapid recovery is why being awake but numb has become the standard of care in advanced ophthalmology.
How Robotic Assistance Improves Precision in Retinal Peeling?
Robotic assistance dramatically improves precision in delicate procedures like retinal peeling by filtering out the natural tremor in a surgeon’s hands and enabling movements at a microscopic scale that are beyond human physical capability. This technology acts as a seamless extension of the surgeon’s skill, translating their intent into flawlessly steady, sub-millimeter motions. While not yet standard for most glaucoma surgeries, it represents the pinnacle of procedural control in ophthalmology.
The retina is an incredibly delicate structure, with layers thinner than a human hair. Procedures like an epiretinal membrane peel require the surgeon to grasp and remove a transparent film of scar tissue from the retinal surface without causing damage. The challenge is immense. A robotic surgical system uses advanced software and mechanics to create a stable, tremor-free environment. The surgeon, often looking through a high-magnification microscope, controls robotic arms that hold microscopic instruments.
This system provides a level of precision that is transformative. It allows for more consistent and repeatable outcomes, potentially reducing surgical time and minimizing the risk of iatrogenic damage to the fragile retinal tissue. The technology embodies the core philosophy of modern surgery: maximizing control to enhance patient safety and improve visual results, especially in the most complex and delicate cases.
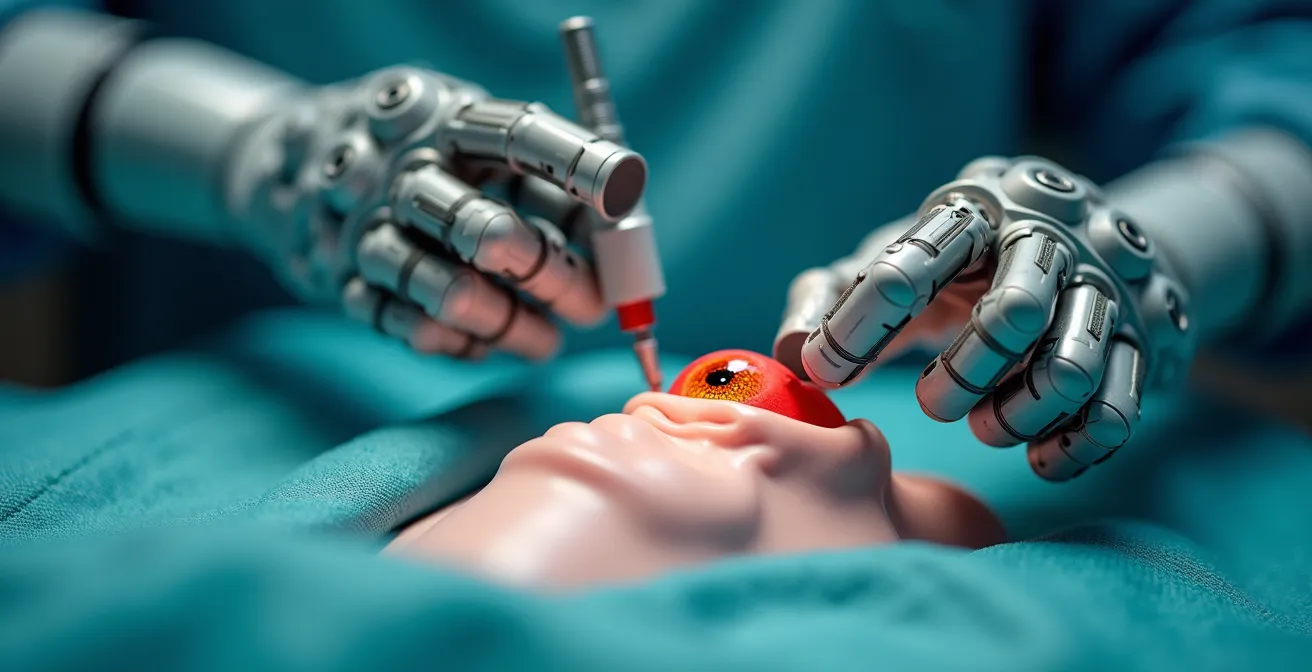
As this image illustrates, the fusion of human expertise and robotic stability allows for an unprecedented level of finesse. This pursuit of micro-surgical precision is a theme that echoes across all advanced ophthalmic interventions, from retinal work to the fine-tuned incisions of glaucoma and cataract surgery. It is a powerful reassurance that the tools being used are engineered to operate at a scale that matches the delicacy of the human eye itself.
Injections or Surgery: Which Is Best for a Macular Hole?
The best treatment for a macular hole depends primarily on its size and stage; small, early-stage holes may be monitored or treated with a gas injection in the office, while larger or persistent holes typically require a surgical procedure called a vitrectomy. This decision-making process, balancing a less invasive approach against a more definitive surgical one, is a perfect parallel to the choices patients face in other conditions, like glaucoma.
This same principle of tailored intervention—weighing the benefits and risks of different levels of invasiveness—is central to the glaucoma treatment debate. Patients with mild to moderate glaucoma are often candidates for Minimally Invasive Glaucoma Surgery (MIGS), while those with advanced, rapidly progressing disease may require a more aggressive, traditional trabeculectomy. Understanding the trade-offs is crucial for an informed decision.
The following comparison, based on data from ophthalmic specialists, breaks down the key differences. As you review it, think of it not as a definitive “winner vs. loser” but as a framework for discussing with your surgeon which approach aligns best with your specific disease stage and lifestyle needs, as confirmed by a detailed analysis of surgical options.
| Aspect | MIGS Procedures | Traditional Trabeculectomy |
|---|---|---|
| Recovery Time | Few days to normal activities | Several weeks of rest and monitoring |
| Incision Size | Often smaller than 2 millimeters | Larger openings required |
| Pressure Reduction | Moderate (mid-teens mmHg) | More aggressive reduction |
| Safety Profile | Lower risk of infection and hypotony | Higher risk of complications |
| Best For | Mild to moderate glaucoma | Severe glaucoma threatening sight |
MIGS procedures prioritize safety and rapid recovery, making them an excellent choice for patients whose intraocular pressure (IOP) doesn’t need to be drastically lowered. In contrast, a trabeculectomy offers a more powerful pressure reduction, which is essential for saving sight in severe cases, but it comes with a longer recovery and a higher risk profile. The choice is a calculated one, made between you and your surgeon.
The Endophthalmitis Risk: Why Water Is the Enemy After Eye Surgery
After eye surgery, water is considered the enemy because it can harbor bacteria and other microorganisms that may cause a devastating infection inside the eye called endophthalmitis. A surgical incision, no matter how small, creates a potential entry point for these pathogens. Avoiding contact with non-sterile water from taps, showers, pools, or hot tubs is one of the most critical post-operative instructions to ensure a safe and successful recovery.
Endophthalmitis is a rare but serious complication that can lead to severe vision loss or even loss of the eye itself. The internal environment of the eye is sterile, and its introduction to common bacteria like *Pseudomonas aeruginosa*, often found in water, can trigger a rapid and severe inflammatory response. This is why your surgeon will provide strict guidelines about keeping the eye dry for a specific period after surgery. This isn’t just a casual recommendation; it’s a vital part of your recovery architecture.
While the risk is low, its severity is high, which is why adherence to post-operative care is non-negotiable. This is especially true for more invasive procedures like trabeculectomy, which has a strong track record for efficacy but requires diligent aftercare. According to research from the National Eye Institute, trabeculectomy successfully lowers eye pressure in about 7 out of 10 people, but this success is contingent on preventing complications. Following your surgeon’s instructions is your most important role in the healing process.
Your Post-Operative Glaucoma Surgery Checklist
- Medication Adherence: Use all prescribed eye drops exactly as directed for the full duration to control inflammation and prevent infection. These are different from your regular glaucoma drops.
- Activity Restriction: Avoid all heavy lifting (typically anything over 10-15 lbs), bending at the waist, and strenuous activity for the specified period, usually 2 to 4 weeks.
- Hygiene Protocol: Keep the eye completely dry. Avoid getting water, soap, or shampoo in the eye when showering. Do not swim or use hot tubs.
- Follow-up Commitment: Attend all scheduled post-operative appointments. These check-ups are crucial for monitoring eye pressure and ensuring the surgical site is healing correctly.
- Symptom Awareness: Immediately report any signs of infection—such as increasing pain, redness, discharge, or a sudden decrease in vision—to your doctor’s office.
Problem & Solution: Surviving “Face-Down” Recovery Without Neck Pain
For certain retinal surgeries, such as those for a macular hole or detached retina, a “face-down” or prone positioning is required for several days to a week. This is necessary to allow a gas bubble, placed in the eye during surgery, to press against the retina and act as an internal bandage. The problem is that maintaining this position is physically and mentally taxing, often leading to severe neck, back, and shoulder pain. The solution lies in a combination of specialized equipment and strategic planning.
Instead of improvising with stacks of pillows, patients can rent or purchase vitrectomy recovery equipment designed specifically for this purpose. This includes cushioned face cradles that attach to a table or bed, allowing you to breathe and communicate while keeping your head in the correct position. There are also chairs that support your body in a seated, face-down posture, as well as mirrors that allow you to see forward while looking down, enabling you to watch television or interact with family.
Planning is equally important. Prepare your living space beforehand. Set up “stations” for eating, sleeping, and entertainment that are all compatible with the face-down position. Break up the day into manageable chunks, alternating between different positions (e.g., sitting in a vitrectomy chair, lying on a bed with a face cradle) to reduce strain on any one part of your body. This turns the recovery from an endurance test into a manageable, albeit inconvenient, phase of healing.

Creating a serene and functional recovery environment, as shown here, is key to minimizing stress and discomfort. This proactive approach to “recovery architecture” transforms a daunting requirement into a structured, survivable process. It’s another example of how the modern surgical ecosystem extends far beyond the operating room to support the patient through every stage of their journey back to health.
Non-Proliferative or Proliferative: Which Stage Requires Laser Treatment?
In diabetic retinopathy, the proliferative stage is the one that typically requires laser treatment. In the earlier, non-proliferative stage, damaged blood vessels in the retina leak fluid but there is no new, abnormal vessel growth. However, in the proliferative stage, the retina begins growing fragile, abnormal new blood vessels (neovascularization) in response to poor circulation. These vessels can bleed into the eye or cause tractional retinal detachment, leading to severe vision loss, and pan-retinal photocoagulation (PRP) laser is used to stop their growth.
This concept of disease staging—identifying the severity and characteristics of a condition to apply the right level of intervention—is a universal principle in medicine, and it is especially critical in glaucoma management. Just as a surgeon wouldn’t use aggressive laser treatment for mild, non-proliferative retinopathy, they tailor the surgical approach for glaucoma based on its stage. This is where the distinction between MIGS and trabeculectomy becomes most clear.
Case Study: The Role of a MIGS Device (Trabectome)
A study by Maeda and colleagues on the standalone use of the Trabectome, a MIGS device, provides a clear example of targeted intervention. In 80 eyes with a high average preoperative IOP of 26.6 mmHg, the procedure successfully reduced the pressure to 17.4 mmHg six months later. Importantly, it also reduced the burden of medication, with patients decreasing from an average of 4.0 eye drops to 2.3. This demonstrates how a micro-invasive approach can achieve a meaningful, moderate pressure reduction for appropriate candidates.
However, this moderate reduction is not always enough, particularly for patients with advanced damage who need much lower eye pressures to halt vision loss. This is the crucial trade-off. As one of the most respected glaucoma research organizations points out, a more aggressive approach is sometimes unavoidable.
Although the majority of MIGS procedures are safer than trabeculectomy, they are also not as effective in lowering eye pressure. The eye pressure in the majority of MIGS clinical trials is typically in the mid-teens range (approximately 15 mmHg). Many ophthalmologists do not think MIGS procedures are appropriate for patients who have advanced glaucoma and need much lower eye pressures.
– BrightFocus Foundation, Minimally Invasive Glaucoma Surgeries Guide
Femtosecond Laser or Manual Incision: Is the Extra Cost Worth the Precision?
Whether the extra cost of a femtosecond laser over a manual incision is “worth it” depends on the specific surgical goal and patient anatomy, as both methods yield excellent results in the hands of a skilled surgeon. A femtosecond laser offers automated, computer-guided precision for creating perfectly circular and centered openings in the lens capsule and making corneal incisions. A manual incision relies on the surgeon’s expert hand-eye coordination. For many routine cases, the added precision of the laser may not translate to a clinically significant difference in visual outcome.
However, in complex cases—such as with a very dense cataract, a weak lens capsule, or certain types of astigmatism—the reproducible precision of the laser can provide an added margin of safety and predictability. It automates some of the most technically demanding steps of cataract surgery, potentially reducing ultrasound energy needed to remove the lens and leading to less inflammation post-operatively.
This entire debate over advanced technology versus proven traditional techniques mirrors the conversation in the glaucoma space. The goal is always to achieve the desired outcome while minimizing risk. For instance, the landmark Tube Versus Trabeculectomy (TVT) Study directly compared two traditional but different approaches for advanced glaucoma. The findings showed that while both were effective, their complication profiles differed, with early complications seen in 21% of the tube group versus 37% of the trabeculectomy group. This kind of data helps surgeons weigh the risk-benefit profile for each individual, just as they do when deciding between a laser and a manual blade.
Ultimately, the most important factor is the surgeon’s experience and judgment. The choice between femtosecond laser and manual techniques, like the choice between different glaucoma procedures, is about selecting the right tool for the right job to ensure the highest likelihood of a safe and successful outcome.
Key Takeaways
- The decision between MIGS and trabeculectomy is not a simple choice but is based on a careful staging of your specific glaucoma severity.
- Modern anesthesia allows for safe, pain-free surgery while you are awake, leading to a much faster and more comfortable recovery.
- Advanced technologies like robotics and lasers are part of a larger surgical ecosystem designed to maximize precision, control, and patient safety.
Open-Angle or Closed-Angle: Which Glaucoma Type Is a Medical Emergency?
Acute angle-closure glaucoma is a clear medical emergency, whereas open-angle glaucoma is a chronic, slowly progressing condition. In an acute angle-closure attack, the drainage angle inside the eye becomes physically blocked, causing a rapid and painful spike in intraocular pressure (IOP) that can destroy the optic nerve and cause permanent blindness in hours if not treated immediately. Symptoms are severe and sudden: intense eye pain, headache, nausea, blurred vision, and halos around lights.
In contrast, open-angle glaucoma, the most common form, is insidious. The drainage angle is open, but the trabecular meshwork (the eye’s drain) gradually becomes less efficient over many years. The rise in IOP is slow and painless, and there are no early symptoms. Vision loss starts in the periphery and goes unnoticed until the damage is significant and irreversible. This is why it’s often called the “silent thief of sight” and why routine eye exams are so critical.
Understanding this fundamental difference is the final piece of the puzzle. It explains the “why” behind the entire discussion of surgery. For open-angle glaucoma, the goal of interventions like MIGS or trabeculectomy is to control a chronic process and prevent future damage. For acute angle-closure, the immediate goal is to break the attack with medication and laser (iridotomy) to prevent catastrophic vision loss. This knowledge solidifies your understanding of the landscape, empowering you to move from a place of generalized fear to one of specific, actionable knowledge. You are no longer just a patient with “glaucoma”; you are an informed partner in the management of a specific condition.
Now that you are equipped with a deeper understanding of the entire surgical ecosystem, the next logical step is to channel this knowledge into a focused and productive consultation. Prepare your questions, articulate your concerns, and work with your surgeon to co-design the treatment plan that gives you the greatest confidence.
Frequently Asked Questions About Glaucoma Surgery Options
Are MIGS procedures safer than traditional trabeculectomy?
Overall, MIGS procedures are considered safer than traditional trabeculectomy or tube shunt surgeries because they have a lower risk of certain complications, such as excessively low eye pressure (hypotony) or infections related to the surgical site (bleb infection).
Is there long-term data on MIGS effectiveness?
As a newer class of procedures, MIGS does not yet have the same decades of long-term data on safety and effectiveness that exist for trabeculectomy. Currently, there are no completed randomized clinical trials directly comparing most MIGS procedures to the “gold standard” trabeculectomy.
Can having a MIGS procedure prevent me from having traditional surgery later if I need it?
No, undergoing a MIGS procedure does not prevent you from having a more traditional surgical approach, such as a trabeculectomy or a tube shunt, in the future if your glaucoma progresses and requires a more aggressive intervention.