Types of vision correction
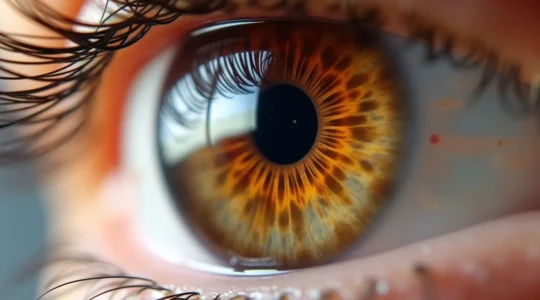
Clear vision shapes how we experience the world, yet millions of people live with refractive errors, cataracts, or complex corneal conditions that blur their daily lives. The field of vision correction has evolved dramatically, offering a spectrum of options that range from simple contact lenses to sophisticated microsurgical interventions. Understanding these different approaches—and knowing which might be right for your specific situation—can feel overwhelming when you’re faced with unfamiliar terminology and life-changing decisions.
This comprehensive resource breaks down the major categories of vision correction, explaining how each method works, who benefits most, and what realistic outcomes you can expect. Whether you’re exploring your first pair of contact lenses, considering laser surgery, or navigating a diagnosis that requires specialized treatment, you’ll find the foundational knowledge you need to approach these decisions with confidence and clarity.
Understanding the Spectrum of Vision Correction
Vision correction isn’t a one-size-fits-all proposition. Your eyes are as unique as your fingerprints, and the optimal solution depends on multiple factors: the specific refractive error you have, the health of your cornea and retina, your age, lifestyle demands, and even your willingness to accept certain trade-offs. Think of vision correction as a toolkit—some tools are designed for precision work on specific problems, while others offer versatile solutions for common issues.
The correction methods available today fall into three primary categories: surgical interventions that permanently reshape the eye’s optical system, contact lenses that provide flexible, reversible correction, and alternative or specialty approaches for eyes that don’t respond well to conventional treatments. Each category contains multiple options, and recent technological advances continue to expand what’s possible for even the most challenging visual conditions.
Surgical Vision Correction: Permanent Solutions
Surgical approaches represent the most definitive path to vision correction, offering permanent or long-lasting changes to your eye’s structure. These procedures have become remarkably refined, with success rates that have made them among the most commonly performed operations worldwide. However, permanence cuts both ways—while you gain freedom from glasses or contacts, you also accept changes that typically cannot be reversed.
Refractive Surgery for Common Vision Problems
Laser refractive surgery—including LASIK, PRK, and newer surface ablation procedures—works by precisely reshaping the cornea to correct nearsightedness, farsightedness, and astigmatism. The principle is elegant: by removing microscopic amounts of corneal tissue in a calculated pattern, surgeons alter how light bends as it enters your eye. A person with moderate myopia might have corneal tissue thinner than a human hair removed, yet this tiny change can eliminate the need for glasses entirely.
Not everyone qualifies as an ideal candidate, however. Age impacts candidacy significantly—surgeons typically recommend waiting until your mid-twenties when prescriptions stabilize, and presbyopia (age-related near vision loss) becomes a factor after forty. Corneal thickness, existing dry eye conditions, and the stability of your prescription all influence whether you’re a good match for these procedures. Pre-existing dry eye, in particular, requires careful management before surgery, as the procedure temporarily disrupts corneal nerve function and can worsen symptoms.
The first twenty-four hours after refractive surgery are critical for healing. Most patients experience blurry vision, light sensitivity, and a gritty sensation as the corneal surface regenerates. Following positioning instructions and using prescribed drops correctly during this window significantly impacts your final outcome and comfort during recovery.
Cataract Surgery: Restoring Clarity
When the eye’s natural lens becomes cloudy—a condition called cataracts—surgical lens replacement becomes necessary to restore vision. This is distinct from refractive surgery; cataract procedures address a structural opacity rather than reshaping focusing power. During the operation, the clouded lens is broken up (often using ultrasound or laser assistance) and replaced with a clear artificial intraocular lens.
The question “when should I have cataract surgery?” depends less on calendar timing than on functional impact. Delaying surgery too long can actually increase complications, as advanced cataracts become harder and denser, requiring more ultrasound energy to remove and potentially causing more inflammation. Yet rushing into surgery before cataracts meaningfully impair your daily activities isn’t necessary either. The right timing balances surgical risk against quality-of-life concerns like difficulty with night driving, trouble reading, or challenges with activities you enjoy.
Interestingly, cataracts don’t develop uniformly across all populations. Climate plays a documented role—people living in high-UV environments or at higher altitudes tend to develop cataracts earlier and faster than those in temperate regions. This environmental factor underscores the importance of UV protection throughout life as a preventive measure.
Retinal and Specialized Microsurgery
When vision problems stem from the retina rather than the eye’s focusing system, highly specialized interventions become necessary. Conditions like retinal detachment, macular holes, diabetic retinopathy, or vitreous hemorrhage require precision microsurgery that operates on structures measured in micrometers. These procedures—including vitrectomy (removal of the eye’s gel-like vitreous) or direct retinal repairs—demand an entirely different skill set and technological approach than anterior segment surgery.
Retinal surgery often requires specific anesthesia protocols, as the eye must remain perfectly still during delicate maneuvers. Recovery can be demanding; some procedures require strict head positioning for days or even weeks afterward to ensure proper healing. The risk of post-surgical infection, while low, carries particularly serious consequences in retinal surgery, making meticulous post-operative care essential.
Emerging technologies like surgical robotics are beginning to enter the operating room, offering surgeons enhanced precision for the most complex retinal cases. While still developing, these systems promise to push the boundaries of what’s treatable, particularly for conditions affecting the macula—the retina’s high-resolution center.
Contact Lenses: Flexible Vision Correction
For those seeking reversible correction or who aren’t surgical candidates, contact lenses offer remarkable versatility. Modern lens materials and designs can address nearly every refractive error, from simple myopia to complex corneal irregularities that defy conventional correction.
Standard Soft Lenses vs. Specialty Options
Conventional soft contact lenses work beautifully for straightforward prescriptions—simple nearsightedness or farsightedness without significant astigmatism. They’re comfortable, affordable, and available in convenient daily disposable formats that minimize infection risk and maintenance hassle. However, their flexibility becomes a limitation when precise optical performance is required.
For irregular corneas—whether from keratoconus, post-surgical changes, or scarring—specialty lens designs become essential. Scleral lenses, which vault over the cornea and rest on the white of the eye, create a fluid reservoir that effectively neutralizes corneal irregularities. Hybrid lenses combine a rigid gas-permeable center (for optical clarity) with a soft peripheral skirt (for comfort), offering what many consider the best of both worlds.
Correcting Astigmatism with Toric Lenses
Astigmatism—caused by an oval-shaped cornea rather than a spherical one—requires lenses with different powers in different meridians. Standard soft lenses tend to rotate on the eye, causing the correction to misalign and resulting in blurred, fluctuating vision. Toric lenses incorporate stabilization features (like weighted zones or thin areas) that keep them properly oriented.
Proper insertion technique matters significantly with toric lenses. The lens must align with your astigmatism axis—imagine trying to correct vision through glasses tilted at the wrong angle. Many people with high astigmatism struggle with standard soft torics and achieve better results with custom soft lenses or rigid gas-permeable designs, which maintain their shape on the eye and provide crisper optics, particularly for night driving.
One critical warning: never purchase “compatible” prescription lenses online without proper fitting. Contact lenses are medical devices requiring specific measurements of your eye’s curvature, diameter, and health status. An improperly fitted lens can cause corneal damage, infections, or vision problems that aren’t immediately obvious until harm has occurred.
Advanced Contact Lens Solutions
Some corneas simply reject laser treatment—whether due to thin corneas, irregular topography, or previous complications. For these patients, advanced contact lens fitting becomes the primary path to functional vision. Custom soft lenses can be designed with unique parameters matching your eye’s specific topography, while scleral lenses can achieve visual stability even with significant corneal irregularity that would be impossible to correct surgically.
The fitting process for these specialty lenses requires expertise and patience. Unlike grabbing soft lenses off the shelf, custom fitting involves detailed corneal mapping, trial lenses, and often multiple adjustments to optimize both comfort and vision. The investment in time and cost typically pays dividends in visual quality that standard options simply cannot provide.
Non-Surgical and Alternative Methods
Beyond mainstream surgery and contact lenses, several alternative approaches deserve consideration, particularly for people seeking to avoid or postpone more invasive interventions. Orthokeratology uses specially designed rigid lenses worn overnight to temporarily reshape the cornea, providing clear daytime vision without lenses or surgery. While the effect reverses when you stop wearing the lenses, this appeals to people who want vision correction without permanent changes or daytime lens wear.
Low-vision rehabilitation takes a different approach entirely, using magnification, contrast enhancement, and adaptive strategies to maximize remaining vision when medical treatment has reached its limits. For conditions like advanced macular degeneration or glaucoma, these techniques can preserve independence and quality of life.
Certain pharmaceutical approaches—particularly injection therapy for retinal conditions like wet macular degeneration or diabetic macular edema—don’t “correct” vision in the traditional sense but prevent further loss. The choice between vitrectomy and injection therapy for these conditions depends on the specific pathology, with injections offering a less invasive approach for many patients.
Choosing the Right Vision Correction for Your Needs
With so many options available, how do you navigate toward the right choice? Start by getting a comprehensive eye examination that goes beyond just measuring your prescription. Understanding the health of your cornea, lens, and retina provides the foundation for appropriate recommendations.
Consider your lifestyle demands honestly. A commercial airline pilot faces different visual requirements than a office worker, just as a competitive swimmer needs different solutions than someone who rarely gets their face wet. Think about your comfort with risk and permanence—some people value the security of reversible options, while others prioritize the freedom from daily lens routines.
Financial considerations extend beyond initial costs. While refractive surgery involves significant upfront expense, the lifetime cost of contact lenses and solutions may actually exceed surgical fees over several decades. Some surgical centers offer lifetime enhancement guarantees, while others charge for any future adjustments. Understanding the true long-term investment helps you make economically sound decisions.
Finally, timing matters more than many realize. Major life events—pregnancy, career changes, relocations—can impact both your ability to manage recovery and your visual needs. Planning vision correction around these transitions, rather than during them, typically leads to better experiences and outcomes.
The landscape of vision correction continues to evolve, offering increasingly sophisticated solutions for even the most challenging visual conditions. By understanding the fundamental categories, recognizing what makes you a good candidate for specific approaches, and asking informed questions of your eye care team, you can navigate these options with the confidence that comes from genuine knowledge rather than marketing promises.
Toric Contacts or Glasses: Which Provides Better Stability for High Astigmatism?
For patients with high astigmatism, achieving consistently sharp vision depends less on the device itself and more on its rotational stability on the eye. Standard soft toric lenses can rotate with blinks, causing intermittent blur, a problem that intensifies with…
Read more
LASIK vs. PRK vs. SMILE: A Surgeon’s Guide to Recovery Time & Returning to Work
While LASIK offers the fastest “wow” factor in vision recovery, SMILE provides a comparable rapid return to life with potentially fewer long-term dry eye complications, making it a powerful choice for professionals. LASIK’s immediate clarity comes from creating a corneal…
Read more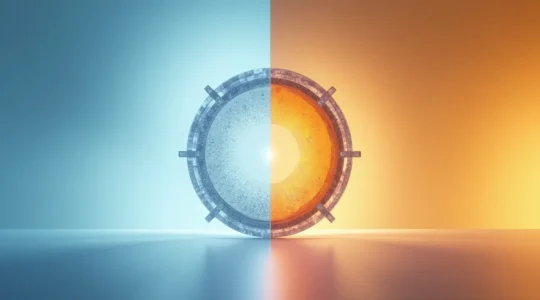
Phakic Implants or Clear Lens Exchange: What Is Best for High Hyperopia?
For high hyperopia (+6.00) patients disqualified from LASIK, the best solution isn’t a single procedure but one that matches your eye’s unique structural blueprint. Phakic IOLs (like ICLs) preserve your natural lens and can offer superior visual quality, making them…
Read more
MIGS or Trabeculectomy: Which Glaucoma Surgery Offers Faster Recovery?
The choice is not just MIGS vs. Trabeculectomy; it’s about understanding the entire surgical ecosystem designed for your safety and recovery. Modern eye surgery relies on patient-centric anesthesia, allowing you to be awake but comfortable for a quicker, safer recovery….
Read more
Monofocal or Multifocal IOLs: Which Lens Is Best for an Active Retiree?
The decision between monofocal and multifocal lenses isn’t about finding the “best” technology, but about understanding which lens’s inherent compromises best match your personal lifestyle and visual priorities. Monofocal lenses offer the sharpest possible vision at one distance, typically covered…
Read more